Left Ventricular Assist Devices (LVADs) are changing the game in heart failure treatment. Heart failure affects over 6 million Americans, with about 580,000 in stage D, the most severe1. This shows how badly we need new treatments2.
LVADs are a big step forward in treating heart failure. They help when other treatments don’t work. Sadly, only about 5,000 heart transplants happen each year, leaving a huge gap2.
LVADs are more than just a stopgap. They help patients wait for a transplant by keeping them strong and alive2. This technology has greatly improved the outlook for those with severe heart failure.
Key Takeaways
- LVADs provide life-extending treatment for advanced heart failure patients
- Over 6 million Americans suffer from heart failure
- Traditional treatments often fall short for stage D heart failure
- LVADs serve as a critical bridge to potential heart transplantation
- Technological advancements continue to improve LVAD effectiveness
Understanding Heart Failure and the Need for LVADs
Heart failure is a big problem in the US, affecting millions. New tech has changed how we treat it, especially for stage D heart failure3. Today, 5.7 million Americans have it, and by 2030, it’s expected to hit over 8 million3.
The Growing Impact of Heart Failure
Heart failure is getting worse, making it a big medical issue. Here are some important facts:
- It affects about 5 million people in the US4
- Every year, 58,309 people die from it4
- About 40% of patients die within a year of being diagnosed4
Why Traditional Treatments Fall Short
Old treatments don’t work well for advanced heart failure. Stage D patients have very low survival chances. Traditional treatments don’t offer much hope3.
The Evolution of LVAD Technology
LVAD technology has changed heart care a lot. It started with early devices and now we have modern continuous flow models. These new pumps have greatly improved survival rates, with over 80% of patients living past a year since 20013.
The growth of LVAD tech brings hope to those with advanced heart failure. It offers better survival chances and a better life quality4.
Life-Saving Technology: How LVADs Are Transforming Heart Failure Treatment
Left Ventricular Assist Devices (LVADs) are a major leap forward in treating heart failure. They give new hope to those with serious heart problems. These devices have greatly increased survival rates for heart failure patients, offering a chance to live longer5.
LVAD technology has shown huge success in clinical trials. The REMATCH trial found that LVADs doubled the 1-year survival rate for very sick heart failure patients. This is a huge step forward in heart care, giving patients a second chance at life and better quality of life5.
- Doubled 1-year survival rates for critical heart failure patients
- Extended life expectancy beyond traditional treatment methods
- Reduced mortality for patients with end-stage heart disease
Patients with LVADs see big benefits. The technology gives a lifeline to those with few other options. It acts as a bridge to a heart transplant and as a long-term solution. Studies show that 80-85% of patients live one year after getting an LVAD, and 70-75% make it to two years6.
“LVADs are not just a medical device; they are a beacon of hope for patients facing critical heart conditions.” – Cardiac Research Institute
While LVAD treatment is a huge medical win, it also comes with big costs. The first implant can cost a lot, with average hospital bills of $210,1875. But, the chance to save and improve lives makes it a vital part of modern heart care.
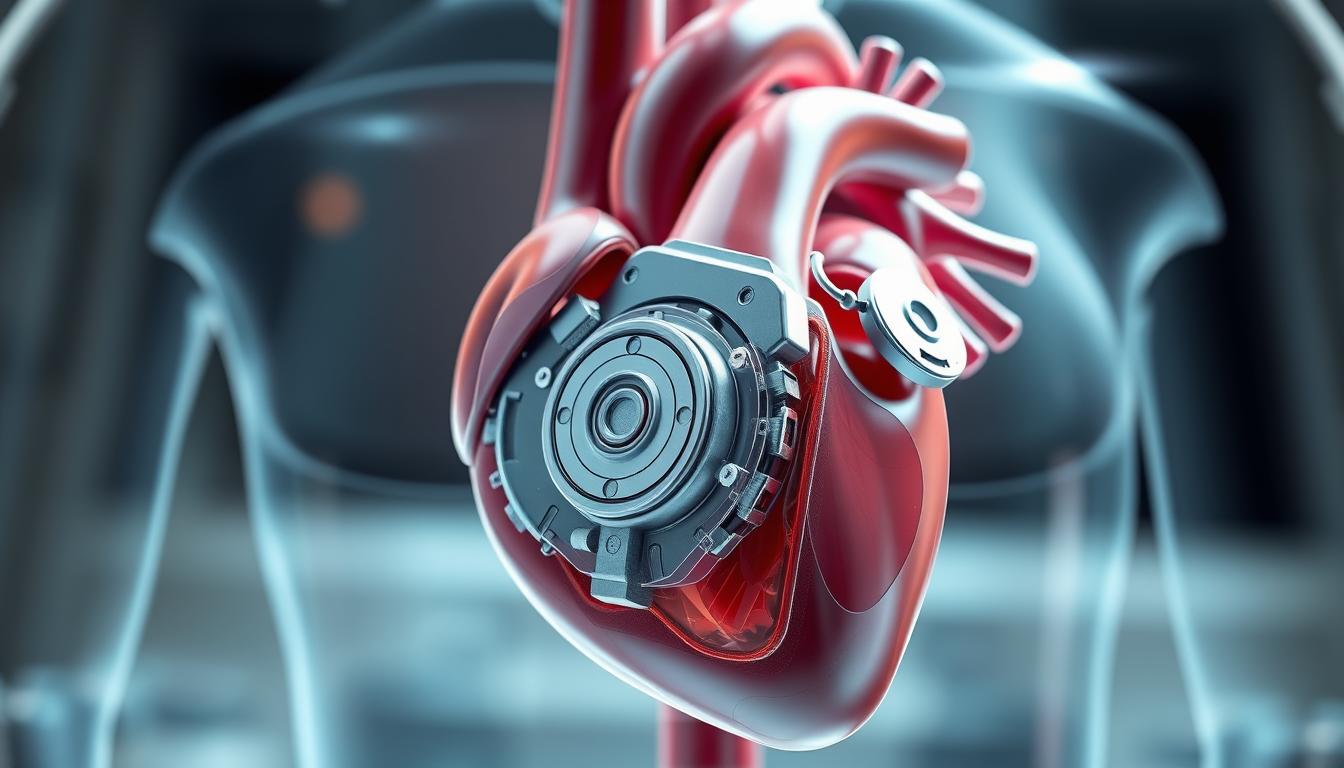
Components and Functionality of Modern LVADs
Left Ventricular Assist Devices (LVADs) are advanced medical tools for heart failure patients. They have complex parts inside and outside to keep blood flowing1.
Internal LVAD Components: The Heart of the System
Modern LVADs have key parts inside that work together to help the heart:
- Implantable pump
- Inflow cannula
- Outflow graft
The pump is the heart of the LVAD, using magnetic levitation to reduce friction7. In 2022, almost all devices used this technology7.
External Components: Powering the Device
External parts of LVADs are also vital for patient care:
- Controller system
- Portable battery pack
- Driveline connection
These parts help monitor and power the device, keeping it running smoothly.
Blood Flow Maintenance Mechanism
LVADs keep blood flowing with precise design. They ensure blood flows consistently, protecting blood cells7. These devices have very low death rates in the first 30 days1.
“Modern LVADs represent a technological breakthrough in managing advanced heart failure, providing hope for patients with limited treatment options.”
Third-generation LVADs have greatly improved survival rates. Patients live up to 86% of the first year and 64% at five years7.
Patient Selection and Evaluation Process
Choosing the right patients for Left Ventricular Assist Device (LVAD) therapy is key. It’s part of evaluating heart failure and picking advanced treatments. About 62,000 patients could get these therapies each year. But only 10,000 get an LVAD or a heart transplant1.

- Assessment of cardiac function using New York Heart Association (NYHA) Functional Classification
- Evaluation of exercise capacity through peak oxygen consumption (VO2)
- Comprehensive medical history review
- Psychosocial assessment
Important factors include certain health markers. For example, patients not on beta blockers with a peak VO2 of 3 might be good candidates. Other signs like a predicted VO2 of ≤50% and a ventilation/VCO2 slope of >35 also show promise1.
The latest LVADs have shown great results. They have a 30-day death rate of just 5% and a 1-year survival rate of 84%1. Patients who get LVADs can see big improvements. They might even move down 2 to 3 levels in their NYHA functional class1.
The LVAD Implantation Procedure
The LVAD surgery is a complex and life-changing treatment for those with severe heart failure. It uses advanced surgical methods to help hearts that can’t pump blood well8.
Surgical Approaches and Techniques
LVAD implantation is a detailed surgery that takes 4-6 hours8. The main method is a median sternotomy. Surgeons then place the device to help the heart pump.
- Median sternotomy is the primary surgical technique
- Device placement requires exceptional surgical precision
- Cardiopulmonary bypass is often utilized during the procedure
Recovery and Post-Operative Care
After surgery, patients stay in the hospital for 2-4 weeks8. This time is crucial for the device to work right and to watch for any issues.
| Recovery Aspect | Key Considerations |
|---|---|
| Hospital Stay | 2-4 weeks of intensive monitoring |
| Potential Complications | Infections, blood clots, bleeding risks |
| Device Management | Continuous external controller monitoring |
Patients must always carry their device controllers and batteries8. They learn to manage their device, which helps them live better and do things they thought they couldn’t do8.
Successful LVAD implantation depends on multiple factors, including patient health and surgical expertise8.
Managing Life with an LVAD
Living with a Left Ventricular Assist Device (LVAD) means you need to learn a lot. You must understand how to manage your device and take care of yourself. This includes knowing about your medications, blood thinners, and how to keep your device clean9.
Managing an LVAD involves several important steps:
- Medication management: Keep taking heart failure meds9
- Blood thinner protocols: Use blood thinners every day to stop clots9
- Regular blood work monitoring9
- Careful driveline exit site maintenance9
Having an LVAD changes your lifestyle. You can’t drive right away, and you need to follow special hygiene rules9. You can shower once your incision heals, but swimming is still off-limits because of the risk to your device9.
| LVAD Lifestyle Consideration | Recommended Action |
|---|---|
| Fluid Intake | Limit to 2 liters per day10 |
| Blood Thinner Management | Maintain INR between 2-310 |
| Blood Pressure Monitoring | Target mean arterial pressure 60-90 mm Hg10 |
It’s also important to get mental support. You might need a caregiver for a few months after surgery. Mental health checks are key to keeping your emotional well-being in check10.

Researchers are working on making LVADs better. They want to create fully implantable devices that will give you more freedom9.
Clinical Outcomes and Survival Rates
Heart failure treatment has seen a big change with Left Ventricular Assist Devices (LVADs). These devices bring new hope to those with serious heart problems. They have greatly improved survival rates and heart failure outlooks4.
Patient Survival Insights
Recent studies show LVADs are changing how we treat heart failure. The latest LVADs have amazing survival rates:
- 30-day mortality rate of only 5%
- 1-year survival rate of 84%11
- Long-term support suggesting survival greater than 50% at seven years11
Quality of Life Improvements
LVADs do more than just help patients live longer. They also greatly improve their quality of life. Most patients go from severe symptoms to mild or no symptoms after surgery11.
The REMATCH trial showed big results. LVADs doubled the 1-year survival rate from 25% to 51% compared to usual treatments5.
Comparative Treatment Analysis
LVADs are a game-changer compared to old heart failure treatments. They add about 8.6 months to a patient’s life5. Cleveland Clinic Florida has a one-year survival rate after LVAD surgery of over 91%11.
Economic Considerations and Healthcare Impact
Heart failure treatment faces big challenges in managing LVAD costs. The cost of putting in an LVAD is very high for healthcare systems. This includes the cost of the device and the surgery12.
The price for left ventricular assist devices can be between €58,000 and €75,000. The cost of the surgery is about €55,00012.
LVADs bring complex financial issues to healthcare. The total cost for continuous-flow LVADs is US $360,407. This is compared to $62,856 for patients treated without a device, showing an extra cost of $297,55112.
Here are some key points:
- Monthly costs for LVAD patients are about €1,261.
- Costs for hospital visits for LVAD patients are around €8,118.
- LVAD patients have 2.64-3.15 hospital visits per year on average.
Studies show that the cost-effectiveness of LVADs is around €107,600 and $198,184 per quality-adjusted life year (QALY) gained12. This highlights the need to balance medical progress with economic realities in treating heart failure13.
Even with high upfront costs, LVADs offer big health benefits. They can add up to three years of life compared to the best medical care12. This makes them a valuable treatment option, even though they are expensive13.
The economic impact of advanced heart failure treatments extends beyond direct medical costs, influencing patient quality of life and healthcare resource allocation.
As healthcare evolves, new technologies and better ways to choose patients might help with LVAD costs13.
Future Directions in LVAD Technology
Heart failure research is making big strides in mechanical circulatory support. New LVAD technologies are on the way. They promise to change how we care for patients and improve their outcomes7.
- Advanced battery technologies with extended life spans
- Fully implantable wireless devices
- Enhanced hemocompatibility
- Reduced infection risks
LVAD technology has seen big leaps lately. In 2022, fully magnetic levitation devices made up 99.8% of the market, with 2,517 devices implanted7. The latest LVADs have greatly boosted patient survival. Now, 86% of patients live for a year, and 64% make it to five years7.
| Technological Focus | Potential Improvements |
|---|---|
| Battery Technology | Longer-lasting wireless power systems |
| Device Design | Reduced stroke and infection risks |
| Patient Monitoring | Real-time health tracking systems |
Researchers are now looking into new ideas. They want to mix LVADs with regenerative therapies. They also aim to make mechanical circulatory support systems smaller and more efficient. The goal is to give heart failure patients more treatment options and maybe even alternatives to heart transplants3.
The future of LVAD technology looks very promising. Ongoing research aims to make life better for patients. It also hopes to expand what’s possible with mechanical heart support4.
Conclusion
Left Ventricular Assist Devices (LVADs) have changed how we manage heart failure. They are a big step forward in treating severe heart conditions14. With 5.7 million people in the U.S. dealing with heart failure, LVADs offer a new hope14.
LVADs have shown great results, improving survival rates for patients. Studies have seen a big jump in 1-year survival rates, with some pumps reaching an 80% rate14. The REMATCH trial showed a huge increase in survival rates for very sick patients, from 25% to 51% in just one year5.
As we move forward, LVAD technology will keep getting better. Doctors and researchers are working hard to make these devices even more effective. LVADs are leading the way in heart care, offering hope to those with severe heart conditions.
FAQ
What is a Left Ventricular Assist Device (LVAD)?
Who is a candidate for LVAD therapy?
How long can a patient live with an LVAD?
What are the daily challenges of living with an LVAD?
Are there different types of LVADs?
What is the cost of LVAD therapy?
How does an LVAD differ from a heart transplant?
What are the potential risks of LVAD implantation?
Can patients with an LVAD travel?
What is the future of LVAD technology?
Source Links
- Left Ventricular Assist Devices: A Primer For the General Cardiologist – https://pmc.ncbi.nlm.nih.gov/articles/PMC9798797/
- The Life-Saving Job of LVADs | Abbott Newsroom – https://www.abbott.com/corpnewsroom/products-and-innovation/life-saving-jobs-of-lvads.html
- Left Ventricular Assist Device in Advanced Refractory Heart Failure: A Comprehensive Review of Patient Selection, Surgical Approaches, Complications and Future Perspectives – https://pmc.ncbi.nlm.nih.gov/articles/PMC11593065/
- Evolvement of left ventricular assist device: the implications on heart failure management – https://pmc.ncbi.nlm.nih.gov/articles/PMC4984573/
- Left Ventricular Assist Devices as Permanent Heart Failure Therapy: The Price of Progress – https://pmc.ncbi.nlm.nih.gov/articles/PMC1360116/
- Focus on: Left ventricular assist devices – https://www.bhf.org.uk/informationsupport/heart-matters-magazine/medical/lvads
- Advancing LVAD Technology: Overcoming Challenges and Shaping the Future of Mechanical Circulatory Support – https://www.mdpi.com/2077-0383/13/24/7813
- Understanding LVAD Surgery: A Lifesaving Solution for Advanced Heart Failure – https://www.daniamedicare.com/blogs/understanding-lvad-surgery-a-lifesaving-solution-for-advanced-heart-failure/
- FAQ: Living with a Ventricular Assist Device (VAD) – https://www.ucsfhealth.org/education/faq-living-with-a-ventricular-assist-device
- Caring for patients with a left ventricular assist device – https://www.myamericannurse.com/caring-patients-left-ventricular-assist-device/
- Left Ventricular Assist Device Therapy: A Destination Too Rarely Visited – https://consultqd.clevelandclinic.org/left-ventricular-assist-device-therapy-a-destination-too-rarely-visited
- The cost-utility of left ventricular assist devices for end-stage heart failure patients ineligible for cardiac transplantation: a systematic review and critical appraisal of economic evaluations – https://pmc.ncbi.nlm.nih.gov/articles/PMC4229461/
- Economic Issues in Heart Failure in the United States: A Report from the Heart Failure Society of America – https://pmc.ncbi.nlm.nih.gov/articles/PMC9031347/
- Left Ventricular Assist Device in Advanced Refractory Heart Failure: A Comprehensive Review of Patient Selection, Surgical Approaches, Complications and Future Perspectives – https://www.mdpi.com/2075-4418/14/22/2480