Did you know that the microbial community in your body outnumbers your human cells by a 10:1 ratio1? This astonishing fact highlights the intricate connections between your gut and overall health, extending far beyond digestion. The pancreas, often recognized for its role in digestion, also plays a crucial part in hormone production, influencing your brain function in ways you might not realize.
Recent studies reveal that the gut-brain axis significantly impacts metabolic regulation2. The pancreas, through hormones like insulin, regulates not just blood sugar but also interacts with the gut to influence brain activity and metabolism3. This complex interplay is essential for maintaining homeostasis and overall health.
Key Takeaways
- The pancreas has dual roles: aiding digestion and producing hormones that influence brain function.
- Insulin plays a key role in metabolism and interacts with the gut-brain axis.
- Digestive enzymes and hormones create pathways connecting the pancreas and brain.
- Emerging models explain how the pancreas-brain axis affects homeostasis and conditions like diabetes.
- Understanding this axis provides insights into managing metabolic and brain-related disorders.
Introduction to the Pancreas-Brain Connection
Your body’s microbial community is a vast ecosystem, with trillions of microorganisms influencing your health. This intricate network extends beyond digestion, playing a crucial role in how your pancreas communicates with your brain.
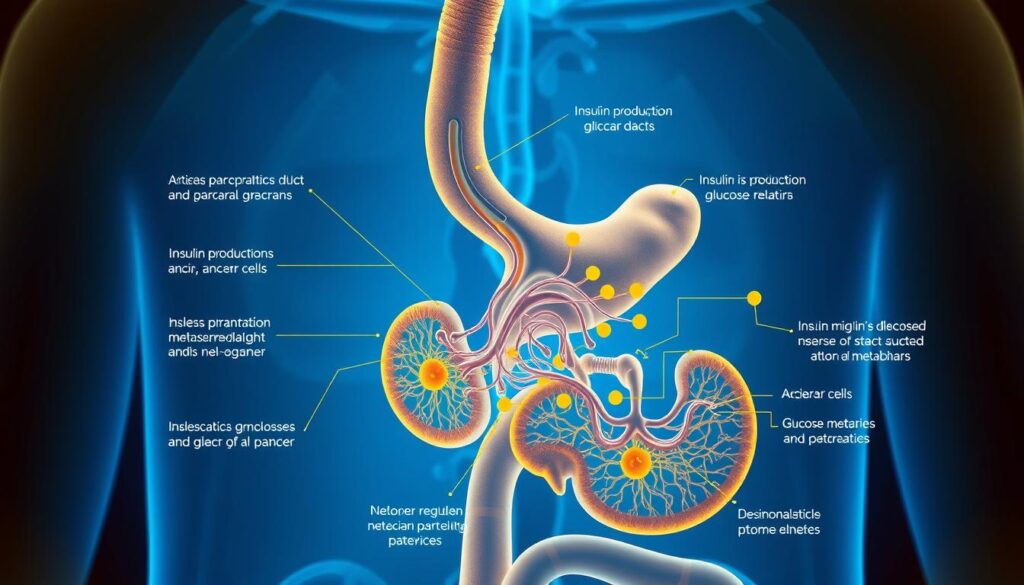
The pancreas is more than just a digestive organ. It produces essential hormones like insulin and glucagon, which regulate blood sugar levels and influence brain activity. This interplay is vital for maintaining balance in your body4.
Specific cells and receptors are the backbone of this communication. The pancreas releases hormones that affect the brain, while the brain sends signals that regulate pancreatic function. This two-way interaction ensures that your body functions smoothly5.
Receptors in the gut and brain work together to support overall function. When these receptors are activated, they trigger responses that maintain homeostasis. This complex system is a key area of study in understanding how the pancreas and brain interact6.
The Fundamental Anatomy of the Pancreas and Brain
Understanding the pancreas and brain connection begins with their anatomy. The pancreas has two main roles: producing digestive enzymes and regulating blood sugar with hormones like insulin and glucagon7. These functions are vital for maintaining balance in your body.
The pancreas is divided into exocrine and endocrine parts. The exocrine part makes enzymes for digestion, while the endocrine part produces hormones. This dual role is crucial for overall health7.
Key Functions of the Pancreas
The pancreas releases hormones that affect both the gut and brain. Insulin and glucagon regulate blood sugar, while other hormones influence appetite and metabolism7.
Neurological Connections Explored
The brain and pancreas communicate through neural pathways. Signals from the brain can trigger the pancreas to release hormones, and hormones from the pancreas can influence brain activity. This two-way interaction is essential for maintaining homeostasis7.
| Function | Description |
|---|---|
| Exocrine Function | Produces digestive enzymes to break down food. |
| Endocrine Function | Releases hormones like insulin and glucagon to regulate blood sugar. |
| Neurological Connection | Communicates with the brain through neural pathways to maintain homeostasis. |
Beyond Digestion: The Pancreas-Brain Axis You Never Knew Existed
Recent have uncovered groundbreaking insights into how the pancreas communicates with the brain, extending far beyond its traditional role in digestion8.
Unlocking Hidden Physiological Pathways
Researchers have discovered that the pancreas uses specific peptides to send signals to the brain, influencing metabolic regulation and appetite control9. These findings challenge our previous understanding of how intake is managed in the body.
One involving rat models revealed that pancreatic peptides can directly affect brain activity related to energy balance10. This research opens new avenues for understanding how intake and metabolism are interconnected through these signals.
Experimental models have also shown that the pancreas and brain communicate through neural pathways, allowing for precise regulation of metabolic functions8. This bidirectional communication ensures that both organs work in harmony to maintain homeostasis.
These discoveries not only deepen our understanding of pancreatic function but also pave the way for future research into therapeutic interventions for metabolic disorders10.
The Dual Role of Digestive Enzymes and Hormones
Discover how your body uses digestive enzymes and hormones to manage food breakdown and nutrient absorption. These processes are vital for maintaining energy balance and overall health.
Digestive Enzyme Functions
Digestive enzymes play a key role in breaking down food into nutrients your body can use. Enzymes like amylase and lipase work in the small intestine to process carbohydrates and fats, ensuring proper nutrient absorption11.
Research using mouse models has shown that these enzymes not only aid digestion but also send signals to the brain. This communication helps regulate appetite and metabolism, linking digestive processes with overall energy balance12.
Endocrine Signaling to the Brain
Hormones like insulin and glucagon, produced by the pancreas, influence metabolism and brain activity. Insulin, for example, regulates blood sugar levels and interacts with the brain to control energy storage and usage13.
Studies highlight how these hormones send specific signals to the brain, affecting how your body manages energy. This endocrine signaling is crucial for maintaining balance and preventing metabolic disorders13.
By understanding how digestive enzymes and hormones work together, you gain insights into the intricate systems that keep your body functioning smoothly. This knowledge can also help in developing new treatments for conditions like diabetes and metabolic syndrome12.
Pancreatic Communication with the Gut
The pancreas and gut interact through complex crosstalk mechanisms that are essential for maintaining digestive health. This communication ensures that both organs work in harmony to support overall well-being.
Crosstalk Mechanisms
The pancreas communicates with the gut through the secretion of enzymes and hormones. These secretions trigger changes in gut functions, such as nutrient absorption and barrier integrity. For instance, proteins like Reg3 and sPLA2 play a crucial role in maintaining the gut barrier, preventing inflammation and infection14.
Neurons also play a vital role in relaying signals between the pancreas and gut. Experimental evidence shows that neural pathways facilitate the exchange of information, ensuring that digestive processes are tightly regulated15.
Maintaining Gut Integrity
Key factors, such as the secretion of specific proteins and neural signaling, ensure the integrity of the gut barrier. This prevents harmful bacteria from entering the bloodstream and causing inflammation. A healthy gut barrier is essential for preventing metabolic disorders and maintaining overall health16.
In summary, the pancreas and gut communicate through a network of secretions and neural pathways. This intricate system maintains the health of the digestive tract and prevents inflammation, ensuring optimal bodily functions.
Immune Interactions and Inflammatory Responses in Pancreatic Function
Discover how your immune system and pancreas work together to protect your gut and regulate inflammation. This intricate relationship is crucial for maintaining your body’s health and preventing diseases like diabetes.
Anti-Microbial Pancreatic Proteins
The pancreas produces special proteins that fight harmful bacteria and pathogens in your gut. These proteins act as a shield, preventing infections and keeping your digestive system healthy. For example, studies show that in 36% of chronic pancreatitis patients, small intestinal bacterial overgrowth (SIBO) is present, highlighting the pancreas’s role in gut protection10.
Inflammatory Signaling in the Gut
Inflammation is a natural response, but too much of it can harm your body. The pancreas helps control this inflammation by sending signals to your gut. When these signals are disrupted, it can lead to an increase in inflammation, which is linked to diabetes and other metabolic disorders10.
Research shows that certain cytokines, like IL-4 and IL-10, are higher in people with chronic pancreatitis. This suggests that the pancreas plays a key role in managing inflammation and keeping your body’s immune response balanced10.
Gut Microbiota and Pathobionts: Impact on Health
Your gut microbiota plays a crucial role in maintaining your overall health by balancing beneficial bacteria and pathobionts. This delicate balance is essential for proper pancreatic function and metabolic regulation.
Role of Beneficial Bacteria
Beneficial bacteria in your gut, such as Bifidobacterium and Faecalibacterium, produce short-chain fatty acids (SCFAs) like butyrate, which are vital for energy metabolism and gut health17. These bacteria help regulate microbial communities and support the integrity of the gut barrier, preventing harmful pathogens from causing inflammation. A healthy gut microbiota also influences hormone production, with hormones like insulin playing a key role in metabolism and pancreatic function.
“A balanced gut microbiota is the cornerstone of a healthy digestive and metabolic system.”
Pathobionts and Disease Links
Pathobionts, such as those from the Enterobacteriaceae family, can lead to various diseases when their numbers are not controlled. Studies show that an overgrowth of these pathogens is linked to conditions like diabetes and metabolic syndrome. For instance, patients with chronic pancreatitis often experience an increase in harmful bacteria, which can disrupt pancreatic function and worsen metabolic disorders17.
| Beneficial Bacteria | Role in Health |
|---|---|
| Bifidobacterium | Produces SCFAs, supports gut barrier integrity |
| Faecalibacterium | Regulates energy metabolism, prevents inflammation |
| Prevotellaceae | Maintains microbial balance, supports immune function |
Disruptions in the gut microbiota can significantly affect pancreatic function and patient outcomes. Clinical studies highlight that restoring this balance through probiotics or dietary changes can improve metabolic health and reduce the risk of diseases associated with the pancreas17.
Mechanisms of Bacterial Translocation to the Pancreas
Bacteria can move from the gut to the pancreas through specific pathways, triggering immune responses that affect pancreatic function. This process, known as bacterial translocation, is a key area of study in understanding gut and pancreatic health.
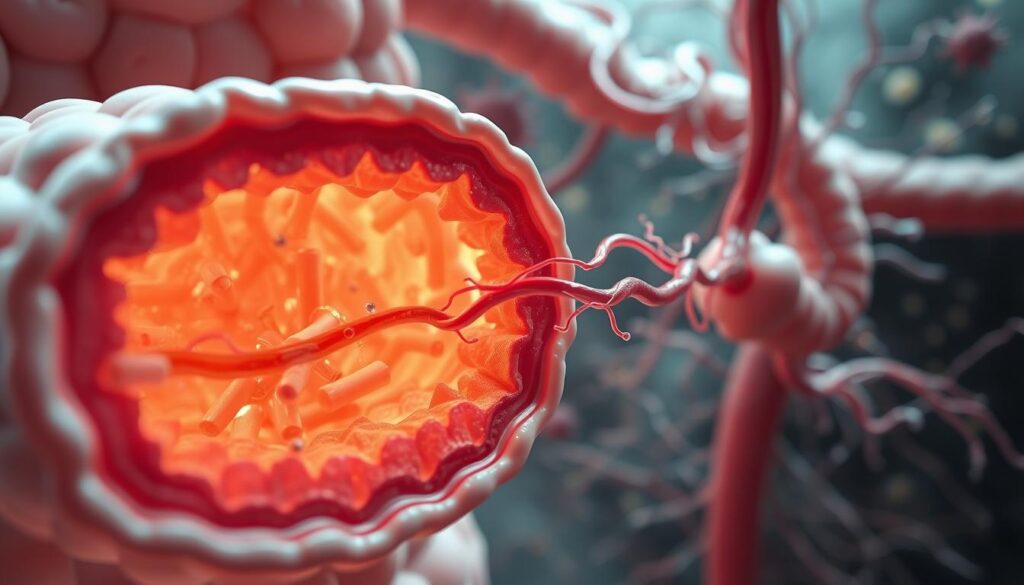
Research shows that bacterial translocation occurs when harmful bacteria cross the gut barrier and reach the pancreas18. This can lead to inflammation and disrupt normal pancreatic activity, including enzyme release and hormone production.
Translocation Routes and Immune Triggers
The primary routes of bacterial translocation include direct invasion through the gut barrier and migration via the bloodstream. Once bacteria reach the pancreas, they trigger an immune response that can lead to inflammation and tissue damage19.
Clinical data reveals that the immune response to translocated bacteria involves the release of specific cytokines, which are signaling molecules that coordinate the body’s defense mechanisms20. This immune response can either protect the pancreas or cause further harm if it becomes excessive.
| Route of Translocation | Immune Trigger |
|---|---|
| Gut Barrier Invasion | Release of pro-inflammatory cytokines |
| Bloodstream Migration | Activation of immune cells in the pancreas |
| Lymphatic System | Stimulation of lymphoid tissues |
Understanding these mechanisms is crucial for developing strategies to prevent harmful bacterial translocation and maintain pancreatic health.
Pancreatic Mediators That Maintain Intestinal Homeostasis
Your pancreas produces specific proteins that help maintain a healthy gut. These proteins play a crucial role in keeping your intestinal environment balanced and free from harmful bacteria.
Reg Family and sPLA2 Effects
The Reg family of proteins and sPLA2 are key players in safeguarding your gut. Studies show that these proteins prevent bacterial overgrowth and maintain the integrity of your intestinal lining4. This helps protect against infections and inflammation.
Research indicates that Reg3 proteins can limit bacterial growth on the intestinal surface, reducing the risk of harmful bacteria entering your bloodstream4. This is especially important for maintaining a healthy balance in your gut microbiota.
Pancreatic Lipase and Gut Balance
Pancreatic lipase, an enzyme produced by your pancreas, indirectly supports gut health. It helps regulate the balance of beneficial and harmful bacteria in your gut4. For example, studies have shown that pancreatic lipase increases the abundance of beneficial bacteria like Akkermansia muciniphila and Lactobacillus reuteri4.
These bacteria are essential for a healthy gut. They help produce short-chain fatty acids (SCFAs), which are vital for energy metabolism and maintaining the integrity of your gut barrier4.
| Mediator | Function |
|---|---|
| Reg Family Proteins | Prevent bacterial overgrowth and maintain gut integrity |
| sPLA2 | Supports antimicrobial activity in the gut |
| Pancreatic Lipase | Regulates gut microbiota balance and promotes beneficial bacteria |
Neural and Hormonal Pathways of the Gut-Brain Axis
The gut-brain axis is a complex communication network that relies on both neural and hormonal pathways to maintain metabolic homeostasis. This system ensures that your body functions smoothly by integrating signals from the gut and brain.
The vagal nerve plays a central role in this communication, transmitting signals from the gut to the brain. Studies show that satiety-associated neurons in the arcuate nucleus are activated in less than 30 seconds after nutrient infusion21. This rapid response highlights the efficiency of neural signaling in energy regulation.
Vagal Nerve Signaling
The vagal nerve is a key player in transmitting gut signals to the brain. It responds to various stimuli, including nutrients and hormones, to regulate appetite and metabolism. For example, hormones like cholecystokinin (CCK) and peptide YY (PYY) induce rapid responses in neurons, helping to control food intake21.
Enteric Nervous System Functions
The enteric nervous system (ENS), often called the “little brain” of the gut, works closely with the vagal nerve. It regulates gut motility and secretion, ensuring proper digestion and absorption of nutrients. The ENS also produces neurotransmitters like serotonin, which influence mood and gastrointestinal function22.
The integration of neural and hormonal signals is crucial for maintaining energy balance. For instance, short-chain fatty acids (SCFAs) produced by gut bacteria enhance the release of gut hormones like GLP-1, promoting insulin secretion and glucose metabolism22. This dual communication ensures that your body efficiently manages energy storage and usage.
“The gut-brain axis is a powerful system that integrates neural and hormonal signals to maintain metabolic homeostasis.”
Clinical studies emphasize the importance of these pathways in overall health. Disruptions in neural signaling can lead to metabolic disorders, while a balanced gut microbiota supports proper hormone production and neural function23. Understanding these interactions provides valuable insights into managing conditions like diabetes and obesity.
Glucoregulatory Peptides in Metabolic Regulation
Glucoregulatory peptides play a vital role in maintaining blood sugar balance and energy levels. These peptides, including oxyntomodulin and glicentin, interact with various metabolic pathways to ensure proper glucose regulation.
Influence of Oxyntomodulin and Glicentin
Oxyntomodulin and glicentin are key players in metabolic regulation. Oxyntomodulin, a peptide hormone, helps regulate appetite and energy expenditure, while glicentin influences insulin secretion and glucose metabolism.
Studies in both human and animal models have shown that these peptides significantly impact insulin sensitivity and glucose homeostasis24. For instance, research indicates that oxyntomodulin enhances insulin sensitivity by promoting glucose uptake in tissues25.
| Peptide | Function |
|---|---|
| Oxyntomodulin | Regulates appetite and energy expenditure |
| Glicentin | Influences insulin secretion and glucose metabolism |
| GLP-1 | Enhances insulin secretion and glucose metabolism |
Clinical data reveal that patients with abnormal glucose metabolism post-pancreatitis often show decreased levels of these peptides26. This highlights the potential for therapeutic interventions targeting glucoregulatory peptides to manage metabolic disorders.
Clinical Insights into Abnormal Glucose Metabolism Post-Pancreatitis
Recent clinical studies have shed light on how pancreatic injury can lead to abnormal glucose metabolism, revealing critical connections between pancreatic health and metabolic disorders. Researchers have identified specific biochemical changes and biomarkers that signal these metabolic shifts, offering new avenues for diagnosis and treatment.
Key Findings from Recent Studies
Chronic pancreatitis, with an annual incidence of 5 to 8 cases per 100,000 adults in the U.S., is closely linked to metabolic disturbances27. Studies show that 38% of patients with chronic pancreatitis develop small intestinal bacterial overgrowth (SIBO), which can further disrupt glucose metabolism27.
Statistical data from clinical studies highlight that patients with acute pancreatitis often experience changes in hormone production. For instance, elevated plasma insulin and glucagon levels at baseline are strong predictors of new-onset prediabetes, with adjusted odds ratios of 1.99 and 3.44, respectively28. These findings underscore the role of hormonal dysregulation in metabolic changes post-pancreatitis.
| Clinical Finding | Statistical Data |
|---|---|
| Incidence of Chronic Pancreatitis | 5 to 8 cases per 100,000 adults annually27 |
| Prevalence of SIBO in CP Patients | 38% of patients27 |
| Predictors of New-Onset Prediabetes | Elevated insulin (OR: 1.99) and glucagon (OR: 3.44)28 |
These studies provide evidence-based insights into the biochemical and hormonal changes following pancreatitis. Such findings support the development of targeted therapies to manage metabolic disorders and improve patient outcomes.
Targeting the Pancreas-Brain Axis for Diabetes Management
Recent advancements in medical research have opened new avenues for managing diabetes by targeting the complex communication network between the pancreas and brain. This approach focuses on modulating both endocrine and neural pathways to achieve better metabolic regulation.
Emerging Therapeutic Strategies
Innovative treatments are now exploring ways to influence the pancreas-brain axis. One promising approach involves GLP-1 receptor agonists, which have shown significant potential in clinical trials. For instance, liraglutide has demonstrated the ability to reduce liver inflammation and improve metabolic markers in patients with non-alcoholic steatohepatitis29.
- GLP-1 agonists enhance insulin secretion and glucose metabolism.
- Devices like the Maestro system use electrical stimulation of the vagus nerve to regulate appetite and metabolism.
- Clinical trials are investigating the efficacy of these treatments in managing type 2 diabetes.
These therapies not only target blood sugar levels but also address the underlying mechanisms that contribute to metabolic imbalances, offering a more comprehensive approach to diabetes management.
Future Research Directions
Future research is expected to delve deeper into the gut-brain axis and its role in metabolic regulation. The gut microbiota produces short-chain fatty acids (SCFAs), which influence hormone secretion and energy balance. Studies have shown that SCFAs like butyrate can enhance insulin sensitivity and regulate appetite30.
- Investigating the impact of SCFAs on pancreatic function and brain activity.
- Developing probiotics that promote beneficial gut microbiota composition.
- Exploring the potential of targeting the MC4R receptor to manage obesity-related diabetes.
These directions highlight the importance of understanding the interplay between the gut, pancreas, and brain in developing effective treatments for diabetes.
The Role of the Gut Microbiome in Energy Metabolism
Energy metabolism is intricately linked to the gut microbiome, which plays a crucial role in how your body processes and utilizes energy. The gut microbiome influences metabolic signaling through various mechanisms, including the production of metabolites that interact with host cells.
Research has shown that individual microbial species within the gut can significantly impact energy metabolism. For instance, certain bacteria produce short-chain fatty acids (SCFAs) such as butyrate, which enhance insulin sensitivity and regulate appetite31. These microbial metabolites initiate signaling actions that regulate the host’s energy balance, ensuring efficient glucose metabolism and energy storage.
Metabolic Signaling and Microbiota
The addition of gut microbiota as a critical factor in comprehensive metabolic health is well-supported by experimental data. Studies indicate that interactions between gut bacteria and host cells have profound effects on metabolic processes. For example, the Microbiome Enhancer Diet (MBD) resulted in an additional loss of 116 ± 56 kcals in feces daily compared to the Western Diet (WD), highlighting the microbiome’s role in energy balance32.
Moreover, the gut microbiota influences nutrient-sensing pathways, with gut hormones such as GLP-1 and PYY playing key roles in maintaining energy homeostasis. This complex interplay underscores the importance of personalized approaches to harness microbial actions for improved health outcomes33.
| Microbial Metabolite | Function in Energy Metabolism |
|---|---|
| Short-Chain Fatty Acids (SCFAs) | Enhance insulin sensitivity and regulate appetite |
| Butyrate | Improves glucose metabolism and energy balance |
| Propionate | Supports satiety and metabolic health |
In conclusion, the gut microbiome’s role in energy metabolism is multifaceted, involving metabolic signaling and interactions with host cells. Understanding and modulating these microbial actions can lead to personalized strategies for enhancing metabolic health and overall well-being.
Innovations in Research and Experimental Models
Recent breakthroughs in experimental models have revolutionized our understanding of pancreas-brain interactions. These innovations are paving the way for new treatments and a deeper comprehension of metabolic regulation.
Animal Studies and Translational Research
Animal models, such as rat and mouse studies, have been instrumental in simulating pancreas-brain interactions. These models reveal how differences in biological processes can translate into human clinical research. For instance, studies show that pancreatic peptides can directly affect brain activity related to energy balance34.
One notable study involving rat models demonstrated that pancreatic peptides influence brain activity linked to metabolism. This research highlights the potential for translational applications in human studies, offering insights into managing metabolic disorders34.
Advances in Clinical Trials
Clinical trials are exploring innovative techniques targeting the nervous system to improve metabolic regulation. For example, GLP-1 receptor agonists have shown promise in enhancing insulin sensitivity and glucose metabolism34.
While some trials have faced challenges, such as variable responses in patient populations, others have achieved significant success. These advancements underscore the evolving nature of research in this complex field.
The integration of animal studies and clinical trials provides a comprehensive approach to understanding pancreas-brain interactions. These efforts emphasize the importance of continued research in developing effective treatments for metabolic disorders.
Conclusion
The intricate relationship between the pancreas and brain plays a pivotal role in maintaining metabolic health, as highlighted throughout this article. Administration of targeted therapies, informed by robust analysis of the pancreas-brain axis, offers promising avenues for managing metabolic disorders4.
Key mechanisms such as insulin regulation and gut-brain signaling are central to this interplay. Research underscores how these pathways influence metabolic control, providing a foundation for future therapeutic strategies35.
Emerging research directions invite exploration into the gut microbiome’s role in metabolic health. This includes the potential of probiotics and dietary interventions to enhance beneficial microbial actions, as evidenced by studies showing increased abundance of probiotics like Akkermansia muciniphila and Lactobacillus reuteri following pancreatic lipase treatment.
In conclusion, comprehensive analysis of the pancreas-brain axis reveals new therapeutic opportunities. By understanding this complex network, we can develop innovative treatments to improve metabolic health and overall well-being.
FAQ
What role does insulin play in the pancreas-brain connection?
How does the pancreas communicate with the brain?
What impact does the gut microbiota have on pancreatic function?
How does the vagus nerve contribute to gut-brain signaling?
What is the significance of glucagon-like peptides in metabolism?
How can targeting the pancreas-brain axis benefit diabetes treatment?
What role do animal models play in pancreas-brain research?
Source Links
- The Second Brain: Is the Gut Microbiota a Link Between Obesity and Central Nervous System Disorders? – https://pmc.ncbi.nlm.nih.gov/articles/PMC4798912/
- Frontiers | Interplay Between the Gut-Brain Axis, Obesity and Cognitive Function – https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2018.00155/full
- Pancreatic endocrine and exocrine signaling and crosstalk in physiological and pathological status – Signal Transduction and Targeted Therapy – https://www.nature.com/articles/s41392-024-02098-3
- Intestinal homeostasis and inflammation: Gut microbiota at the crossroads of pancreas–intestinal barrier axis – https://pmc.ncbi.nlm.nih.gov/articles/PMC9540119/
- Role of the gut–brain axis in energy and glucose metabolism – Experimental & Molecular Medicine – https://www.nature.com/articles/s12276-021-00677-w
- The Brain–to–Pancreatic Islet Neuronal Map Reveals Differential Glucose Regulation From Distinct Hypothalamic Regions – https://pmc.ncbi.nlm.nih.gov/articles/PMC5001176/
- Pancreatic endocrine and exocrine signaling and crosstalk in physiological and pathological status – https://pmc.ncbi.nlm.nih.gov/articles/PMC11825823/
- The enteric nervous system: “A little brain in the gut” – https://www.degruyter.com/document/doi/10.1515/nf-2019-0027/html?srsltid=AfmBOoqsQhE0MFNY46clYnxGWlvmzbPl6z5OwDU6HIBinfeHlP8FRwlO
- Dysregulated brain-gut axis in the setting of traumatic brain injury: review of mechanisms and anti-inflammatory pharmacotherapies – Journal of Neuroinflammation – https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-024-03118-3
- Pancreatitis affects gut microbiota via metabolites and inflammatory cytokines: an exploratory two-step Mendelian randomisation study – Molecular Genetics and Genomics – https://link.springer.com/article/10.1007/s00438-024-02125-6
- Regulation of Pancreatic Secretion (Version 1.0) – https://pancreapedia.org/reviews/regulation-of-pancreatic-secretion-version-10
- The Microbiota–Gut–Brain Axis in Psychiatric Disorders – https://www.mdpi.com/1422-0067/23/19/11245
- Pancreatic regulation of glucose homeostasis – Experimental & Molecular Medicine – https://www.nature.com/articles/emm20166
- Multi-Organ Crosstalk with Endocrine Pancreas: A Focus on How Gut Microbiota Shapes Pancreatic Beta-Cells – https://pmc.ncbi.nlm.nih.gov/articles/PMC8773909/
- The pRb/RBL2-E2F1/4-GCN5 axis regulates cancer stem cell formation and G0 phase entry/exit by paracrine mechanisms – Nature Communications – https://www.nature.com/articles/s41467-024-47680-z
- Frontiers | Kynurenic Acid Acts as a Signaling Molecule Regulating Energy Expenditure and Is Closely Associated With Metabolic Diseases – https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2022.847611/full
- The Kidney–Gut Axis as a Novel Target for Nutritional Intervention to Counteract Chronic Kidney Disease Progression – https://pmc.ncbi.nlm.nih.gov/articles/PMC10819792/
- Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome: A Bridge between Functional Organic Dichotomy – https://www.gutnliver.org/journal/view.html?doi=10.5009/gnl16126
- From the gut to the peripheral tissues: the multiple effects of butyrate | Nutrition Research Reviews | Cambridge Core – https://www.cambridge.org/core/journals/nutrition-research-reviews/article/from-the-gut-to-the-peripheral-tissues-the-multiple-effects-of-butyrate/DADCCD4D5727663E689D30CDE103BBEA
- Microbiota-gut-brain axis: relationships among the vagus nerve, gut microbiota, obesity, and diabetes – Acta Diabetologica – https://link.springer.com/article/10.1007/s00592-023-02088-x
- Frontiers | Enteroendocrine cell regulation of the gut-brain axis – https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2023.1272955/full
- Gut liver brain axis in diseases: the implications for therapeutic interventions – Signal Transduction and Targeted Therapy – https://www.nature.com/articles/s41392-023-01673-4
- The gut microbiota–brain axis in neurological disorder – https://pmc.ncbi.nlm.nih.gov/articles/PMC10436500/
- Glucagon-like peptide 1 (GLP-1) – PMC – https://pmc.ncbi.nlm.nih.gov/articles/PMC6812410/
- The expanding incretin universe: from basic biology to clinical translation – Diabetologia – https://link.springer.com/article/10.1007/s00125-023-05906-7
- Pancreatic regulation of glucose homeostasis – https://pmc.ncbi.nlm.nih.gov/articles/PMC4892884/
- New Insights into Chronic Pancreatitis: Potential Mechanisms Related to Probiotics – https://www.mdpi.com/2076-2607/12/9/1760
- Pancreatic and gut hormones as predictors of new-onset prediabetes after non-necrotising acute pancreatitis: a prospective longitudinal cohort study – https://ec.bioscientifica.com/view/journals/ec/10/7/EC-21-0229.xml
- Gut-Pancreas-Liver Axis as a Target for Treatment of NAFLD/NASH – https://www.mdpi.com/1422-0067/21/16/5820
- Frontiers | The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication – https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2020.00025/full
- The role of probiotics on the roadmap to a healthy microbiota: a symposium report | Gut Microbiome | Cambridge Core – https://www.cambridge.org/core/journals/gut-microbiome/article/role-of-probiotics-on-the-roadmap-to-a-healthy-microbiota-a-symposium-report/249F04E879ED8FB86EED7CDBD0D7B2ED
- Host-diet-gut microbiome interactions influence human energy balance: a randomized clinical trial – Nature Communications – https://www.nature.com/articles/s41467-023-38778-x
- The Microbiota and the Gut–Brain Axis in Controlling Food Intake and Energy Homeostasis – https://www.mdpi.com/1422-0067/22/11/5830
- Whole Alga, Algal Extracts, and Compounds as Ingredients of Functional Foods: Composition and Action Mechanism Relationships in the Prevention and Treatment of Type-2 Diabetes Mellitus – https://www.mdpi.com/1422-0067/22/8/3816
- Frontiers | Guts Imbalance Imbalances the Brain: A Review of Gut Microbiota Association With Neurological and Psychiatric Disorders – https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2022.813204/full